Our internal mechanism of defence (known as the immune system) is made of many different cell types that together help protect us against infections and cancer. Today we are talking (again) about my favourite cell type, called T cell. To do their job, they need to receive specific signals allowing them to be activated and ready to fight the invaders!
But what are those signals? There are three major signals essential for proper T cell activation. The first signal happens following the recognition of the threat (such as a bacteria), and the second and third signals occur primarily due to inflammation. So, for a T cell to go from “I’m just going around your body not doing much” to “I’m ready to fight this threat and WIN” they need those three signals.
But what if our T cells don’t receive all three signals?
Neat question! Let’s say, for example, that you are doing just fine (aka no infection/no cancer/no inflammation). Suddenly, your T cell recognizes its target protein (signal 1) without any “inflammation around”. What now? You are asking the same questions I asked a few years ago, right before I fell in love with T cell tolerance. But before I answer your question, let’s go back to signal 1 for a second. Trust me… you want to stay on for this (learning) ride.
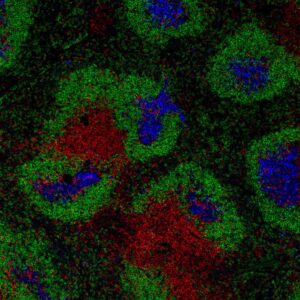
T cells recognize their target protein via a receptor they express on their surface, known as the T cell receptor (or TCR). You might remember from a few posts ago that I explained how our body is able to generate an incredible number of different TCRs (i.e. each will be specific for a different protein, thus recognizing various threats). Dr. Jarrod Dudakov (Immunology Professor, University of Washington) said that some studies have suggested that we can make between 1018 to 1033 possible combinations of TCR. And if you don’t think that it is a lot, “to put that in context, there are about 1018 grains of sand on planet earth”[1]. Mind-blowing, right?!
This MASSIVE number of T cell specificities (due to the different TCRs) is excellent for us to recognize any possible “threats” that we encounter during our lifetime. But here is the catch! This high TCR diversity comes with a cost. Due to the random generation of these receptors, we are now making T cells specific to proteins of our skin, heart, and thyroid… We call these cells self-reactive (or autoreactive) T cells, and they can cause significant health problems.
But wait up because our immune system is smarter than that! And there are many different mechanisms that it implements to keep those cells in check – ensuring they don’t attack our healthy cells. Together, these are called T cell tolerance; you can read more about it here. In this post, we are talking about one of these mechanisms known as T cell anergy.
I’m not responding to this!
The word anergy was first used by Von Pirquet in 1908 to identify a state characterized by an absence of reactivity in the immune system [2]. But around 80 years later, two brilliant scientists, Ronald Schwartz and Mark Jenkins, showed that T cells could become anergic [3]. Wait, what does it mean to be anergic? It means that you are not very responsive to stimuli. Thus instead of being ready to fight, you are “a little lazy about it”.
Remember that to clear a threat, you need T cell strength and numbers! However, T cells that are anergic will have less of their powerful “fighting proteins” (known as cytokines), and they will also proliferate much less than a T cell that is not anergic. Together, this results in “less strength and fewer numbers”. This is a perfect scenario because we DO NOT want T cells that recognize heart proteins to fight and kill our heart cells. That would mean TROUBLE for sure!
So we want our self-reactive T cells to become anergic, meaning when they recognize self-proteins without inflammation, they will be Hyporesponsive (low strength, low numbers) and thus won’t cause damage to our healthy cells.
I’m not lazy, it’s called selective participation
“Wait up Stefanie… why!? Why would our immune system go through the trouble of keeping these self-reactive T cells? Why have a whole mechanism (which is technically much more intricate than what I’m explaining here) to prevent these cells from attacking? Just get rid of these cells!”
Great thinking! Here is another cool thing… everything is about balance. If our immune system just removed all of the cells that it “thinks” would cause us harm (because they react to our self-proteins), we would have a much less diverse T cell repertoire (meaning the T cells with different TCRs). Lowering the diversity would pose a challenge for us because a T cell that is somewhat specific to our heart cell might be REALLY specific to a protein found in a particular virus. And therefore, if we removed this cell, we would have a lower ability to fight cells infected with this virus.
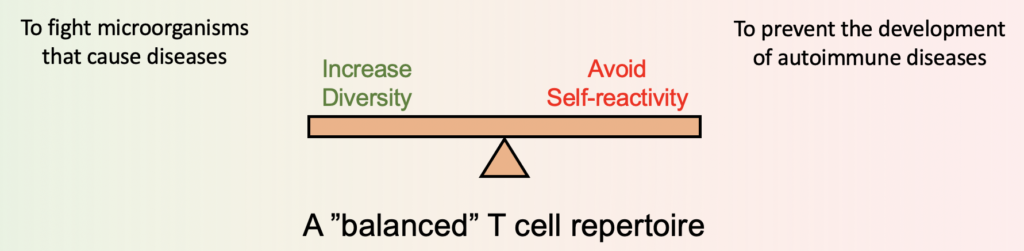
So our immune system “keeps” some self-reactive T cells in this anergic (“lazy”) state to ensure they won’t fight our own cells but could fight other threats. Studies suggest that T cells can reverse their anergic state and be activated and ready to fight when facing a real danger (in our example, if we are infected with that particular virus). Selective participation!
Having this state of “laziness” (or, more scientifically appropriate, hyporesponsiveness), our immune system can keep us healthy while maintaining a very high T cell diversity! Smart, no?! I could talk about T cell anergy (which is also the topic of my PhD project) for a very long time, but I will stop here … for now!
From your immunologists – in training,
Stefanie Valbon
References
[1] from Canadian Society of Immunology Early Career Immunology Seminar Series
[2] Schwartz, R. H. T cell Anergy. Annu. Rev. Immunol. (2003).
[3] Jenkins, M. K. & Schwartz, R. H. Antigen presentation by chemically modified splenocytes induces antigen- specific T cell unresponsiveness in vitro and in vivo. J Exp Medicine 165, 302–319 (1987).