If you are a little bit like me, you have also spent a lot of time trying to figure out how exactly our body is able to function the way it does. Picture this. The immune system is your internal defence mechanism, in order to provide you with the correct level of protection, it needs to know what is “friendly” and what is not. That makes sense, right? But how?
I don’t play online computer games, but my boyfriend, Kevin, does. Every time I see him playing these games, there are usually 50 little avatar people on his computer screen. By some miracle, he knows exactly who is in his team, and who he should attack. If Kevin sent his avatar “killing power” toward his team member, he would, unfortunately, be in a bad position. Killing one of your team members decreases the overall chances of the group surviving. Do you see where I am going with this? EXACTLY, a similar “battle” is going on inside your body.
Think about your body as one team, and everything it wants to remove (such as viruses, bacteria, cancer) in another team. To properly function, your immune system must be able to tell the difference between self (your native cells), from non-self (the other team… pathogens and mutated cells). Cleverly, our immune system implements many levels of protection to ensure that it will keep this difference in check. In this post, I will talk about something that has been on my mind a lot lately, called T cell tolerance!
Self vs Non-Self
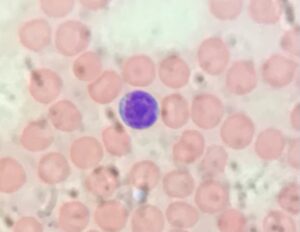
If you remember from my last posts, T cells are immune cells that are part of the adaptive immune system. This system is composed of specialized cells to target a specific portion of the pathogen you are infected with. T cells have different functions in our immune system. They can be considered killer cells, those that kill infected or mutated cells (in the cause of cancer). They can be helper cells, which have many different functions, such as helping other immune cells to function/activate. But T cells can also have regulatory functions, which I will talk more about at the end of this post.
Since T cells are so great at removing/helping to remove a threat, they need to make sure they know the difference between self vs non-self. And this is when tolerance comes in handy! Tolerance is the ability of the immune system to be unresponsive to your native cells. Why? Well, imagine a killer T cell targeting cells of your heart. If this T cell thinks that heart cells are “non-self” it will send all its power to destroy this “invader”. Since your heart is not really an “invader”, this can be very detrimental to you and ultimately cause autoimmune diseases.
Autoimmune disease results from your immune system thinking your own cells (self) are outsiders (non-self). Unfortunately, this can have very bad consequences. Different autoimmune diseases can occur depending on the tissue this defective immune cell attacks.
Now, you must be thinking that most people do not have autoimmune disorders, hence we must have evolved ways to prevent this scenario from occurring. And you are correct! Our immune system has different mechanisms to prevent the generation/ function of such self-reactive T cells.
Central Tolerance
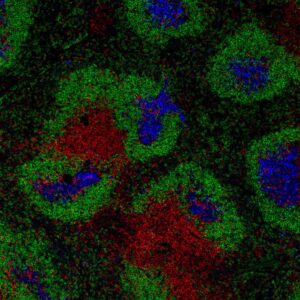
The first layer of protection occurs during T cell development and is called central tolerance. T cells develop in the thymus, the coolest, most amazing organ present in our body (emphasis mine). This organ is located on top of our hearts, and its highly organized structure ensures the proper development of T cells.
T cells possess a receptor called the T cell receptor (or TCR), which is very important to recognize the threat to be removed. Previously, I mentioned how we can generate an extremely high number of TCR specificities (i.e. a TCR specific to a small portion of the influenza virus, a TCR specific to a small portion of SARS-CoV-2, etc). This process, however, can lead to the generation of T cells bearing a TCR specific to a small portion of… heart proteins, for example.
To prevent the release of such harmful cells, T cells will “test” their TCR specificity in the thymus. During this test, if T cells respond strongly to self-proteins, they are deleted. The process is very audacious and involves the expression of a high number of different proteins in the thymus, that otherwise wouldn’t be present. If you want to know more about the process, you should read this great blog post by Inge Wortel.
Central tolerance will ensure that T cells responding very strongly to self-proteins are deleted, become unresponsive, or acquire regulatory functions. However, as we all know, every mechanism can have its difficulties. Since the thymus makes LOTS of T cells every day, maybe a few highly self-reactive T cells will be released from this organ.
Peripheral Tolerance
Our immune system knows that having one layer of protection is never enough. To keep in check any self-reactive T cells that have “escaped” the thymus, the immune system implements a second layer of protection called peripheral tolerance.
Peripheral tolerance occurs outside your favourite organ (i.e. outside the thymus). One way in which peripheral tolerance prevents the harmful effects of self-reactive T cells is by deleting such cells. It can also provide signals that will keep these self-reactive T cells alive but in an unresponsive state, known as anergy. Such T cells might be able to “see” the self-proteins, however, they can’t attack your own cells.
A lot still has to be done to fully understand this anergic state, such as analyzing the exact signals/mechanisms that keep these cells in check. Questions such as “why do we want these anergic cells to remain alive?”, and “do they stay unresponsive forever, or can something trigger their ‘come back’ to a functional state?” are still present in the mind of many scientists (and scientists in the making, like me).
Another mechanism of peripheral tolerance is by generating regulatory T cells (Tregs). Remember when I told you that Kevin knows exactly who to attack when he plays video games? Imagine that if instead of Kevin, it was me playing video games. I AM VERY BAD at video games. I have a very hard time figuring out who is on my team and who is not. My team members would soon realize this “problem” and instead of giving my videogame avatar “killing abilities”, they would kindly ask me to have a different avatar power (so I don’t kill my own team).
A similar process happens with our immune system. Once it recognizes self-reactive T cells in the periphery, it can change them to have regulatory functions (Treg). Tregs have suppressive abilities. They can inhibit many functions of T cells that would cause damage, and therefore these cells are very important for preventing autoimmune diseases.
It is important to note that the generation of Tregs and the establishment of the anergic state can also happen in the thymus, and therefore are also part of the central tolerance. For my PhD project, I’m focusing on understanding different aspects of peripheral tolerance, and that is why I decided to focus on this second section. Keep in mind however that the location (i.e. thymus vs peripheral) is what determines whether we call it central or peripheral tolerance.
How do we fix it?
The problem with autoimmune diseases is the result of our own body “making a mess”, therefore this can make it extra hard for scientists to develop treatments for such diseases. Why? Well, if you have a bacterial infection, you use therapeutics to target the bacteria. However, when you have an autoimmune disease, and you target the immune system, different consequences can occur. Decreasing the function of your immune system can lead you to become more susceptible to infections and cancer, for example. Therefore, we have to think about ways to specifically target the “bad” immune cells, those that are targeting self-proteins, and not to broadly decrease the function of immune cells. And that can be very challenging.
T cell tolerance is the mechanism in which our immune system prevents the generation/function of highly self-reactive T cells, ultimately inhibiting the development of autoimmune diseases. The astonishing balance which allows the generation of T cells specific to many different pathogens, while ensuring they will not attack our own body is one of the reasons why our immune system is so successful!
From your immunologist – in training,
Stefanie Valbon