Do you remember the last time you had to go to a new place but didn’t know the way? You probably had no issue finding the path to reach your expected destination. Today, our phones will act as GPS and provide us with precise directions to go from point A to point B. Easy, right?
But imagine back in time, when people did not have GPS or maps. Everything was slower. Going from point A to B required way more trial and error. Can you think about one thing that should NOT be slow or inaccurate? Exactly, our immune system.
And that is why I picture our immune cells having an internal GPS, which allows them to know exactly where to go. Fast and without mistakes. I wish that our immune cells could say: “Hey Google, where can I find the nearest infected cells?”, unfortunately, that is not the case.
Luckily, our immune system has developed a beautiful and intricate “immune GPS” that allows our cells to sense the environment and migrate from point A to point B whenever necessary. This “immune GPS” is very complex and comprise of many different layers. Today, we will focus on one of its mechanisms, which occurs thanks to a family of proteins called Chemokines. Get ready to be amazed!
How does it work?
To make this concept more palpable, let’s imagine that you were making an apple pie and you cut your finger. A very superficial cut, no big deal, but enough to allow some bacteria to go in. To deal with this threat we need to call the correct immune cells to this site.
But how? Well, it is actually simpler than you think. As I mentioned before, our immune cells can “talk”! Yes, they can. Thanks to a family of proteins called cytokines, our cells are able to send information to one another in any situation. (If you want to know more, check out this post).
A similar mechanism occurs for our “immune GPS”. Chemokines, which are a family of cytokines, provide one of the layers of our GPS. These are small proteins that can be produced by immune and non-immune cells in our body and they serve as signals for cellular migration.
But how can our cells sense this information? Easy! Our cells can express a receptor on their surface, which can detect chemokines. But each type of chemokine can only bind to their specific receptor. Since we have many different types of chemokines, we also must have many different chemokine receptors. Just picture a lock and a key. A specific chemokine (the key) will only bind to a specific receptor (the lock).
Cells will move in response to the amount of chemokine present in a specific location. Chemokines act as Nutella acts for me. The higher the amount of Nutella present in a location, the more I will migrate towards that area. This is “exactly” what is happening with our immune cells. In a site of inflammation, there will be a high concentration of chemokines, and that will attract our immune cells to that location.
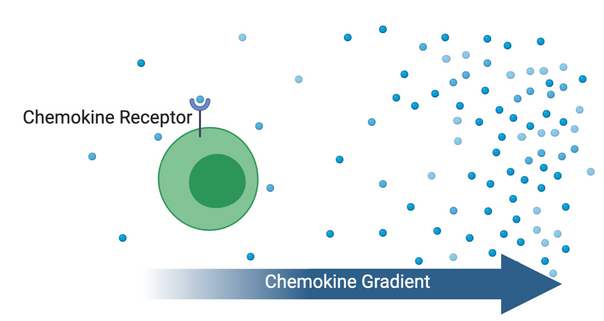
Green cell expresses the receptor specific to the chemokine in the environment (blue dots). Chemokine concentration is lower on the left and higher on the right, creating a chemokine gradient and allowing for cellular migration. Created with BioRender.
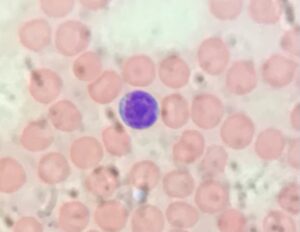
But remember, our immune system is composed of many different cell types, each with specific functions. It would be counter-intuitive to have a system that would bring every single immune cell, every time a threat occurs. So, our system has to somehow “activate” this “immune GPS” only for specific cells, depending on the situation.
This occurs because our cells don’t express all chemokine receptors. Just like not everyone likes Nutella, not every immune cell will have the correct receptor to sense a specific chemokine. Therefore, no matter how much chemokine is present in an environment, if an immune cell doesn’t express the specific chemokine receptor, it won’t move! And this is how our immune system can “tune” the information sent.
What is even cooler is that such chemokine receptors are not fixed on a cell. This means that our cells can regulate the expression of such receptors depending on the situation. For example, if I stop sensing Nutella and start to sense broccoli, I would change my migration pattern towards a location with a high concentration of broccoli (trust me, this is a VERY hypothetical situation).
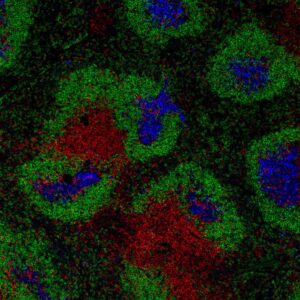
Chemokines are therefore super important to help “organize” the complex network of events occurring inside of us during an infection. But they are also important in many other situations. Another example of chemokine action occurs during the development of my favourite cell (the T cells) inside my favourite organ (the thymus).
Chemokines and T cell development
The thymus (an organ located just on top of our hearts) has a very organized structure and each location is responsible to send specific signals to developing T cells. You can picture this as levels on a videogame. For a T cell to develop completely, it needs to go from level 1 to level 6 (for example). Each level requires a specific signal, which is provided in a specific location inside the thymus.
Once a T cell “upgrades” from level 1 to level 2, it needs to change location, to acquire different information to continue its development. So, at the end of level 1, T cells will start to express a specific chemokine receptor that allows them to sense a chemokine that is highly present where “level 2 developmental signals” are provided. This allows for our T cell to move to the next location to continue its development. Brilliant, right?!
So, next time you wonder how our cells know where to go, trust me, it is not Google showing the way, but small proteins called Chemokines! Thanks for stopping by for one more ImmunoThoughts, keep asking questions and seeking answers!
From your immunologist – in training,
Stefanie Valbon